Healthcare is an essential part of our lives, aimed at preventing diseases, treating conditions, and improving our quality of life. However, in this noble effort to care for our health, healthcare systems can sometimes make errors that result in harm to patients. These errors not only cause physical and emotional suffering but also negatively impact people's trust in the healthcare system. In Latin America and around the world, patient safety has become a critical issue requiring urgent attention. In this blog, we will explore the current landscape of patient safety in Latin America, addressing common challenges and the solutions that organisations can implement to ensure optimal care.
Where Are We in Latin America?
Patient safety is a topic that cannot be overlooked. Harm to patients occurs even in advanced healthcare systems due to increasing complexity and the possibility of human errors. Process errors, lack of communication, and the absence of active patient involvement can be underlying factors in these issues. It is crucial to recognize that solely blaming the active provider does not address latent system errors. Instead of expecting individual perfection, it is necessary to create a safe environment with well-designed systems. This is where a shared and transparent safety culture comes into play, an essential component for preventing and improving healthcare errors.
Patient Safety: What Does It Mean?
Patient safety is not just an abstract concept but a concrete focus in healthcare. As healthcare systems become more complex, the likelihood of risks and errors associated with healthcare increases. The purpose of patient safety is simple yet fundamental: to prevent and reduce hazards, errors, and harm that patients may face during their healthcare. The foundation of this initiative is continuous learning from mistakes and adverse events to continuously improve and evolve.
Latin America: Confronting the Burden of Healthcare-Related Harm
Millions of patients in Latin America experience harm or even die due to unsafe healthcare. The situation is alarming, with examples including medication errors, healthcare-associated infections, and risky surgical procedures. Unsafe practices such as unsafe injections and misdiagnoses contribute to this burden. These problems not only jeopardize patient safety but also affect the overall quality of healthcare in the region.
The Data Speaks for itself
Medication errors result in an annual cost of approximately $42 billion worldwide. Healthcare-associated infections affect 7-10% of hospitalised patients.
Up to 25% of surgical patients experience complications, with one million surgical patients dying annually.
Unsafe injection practices lead to 9.2 million years of disability-adjusted life lost.
Diagnostic errors affect 5% of adults in outpatient care, with more than half of them potentially causing serious harm.
Errors in radiation and septicemia cause preventable harm and deaths.
Venous thromboembolism is responsible for common and preventable harm.
Sources: WHO, IBEAS Study, IBEAS, OPS
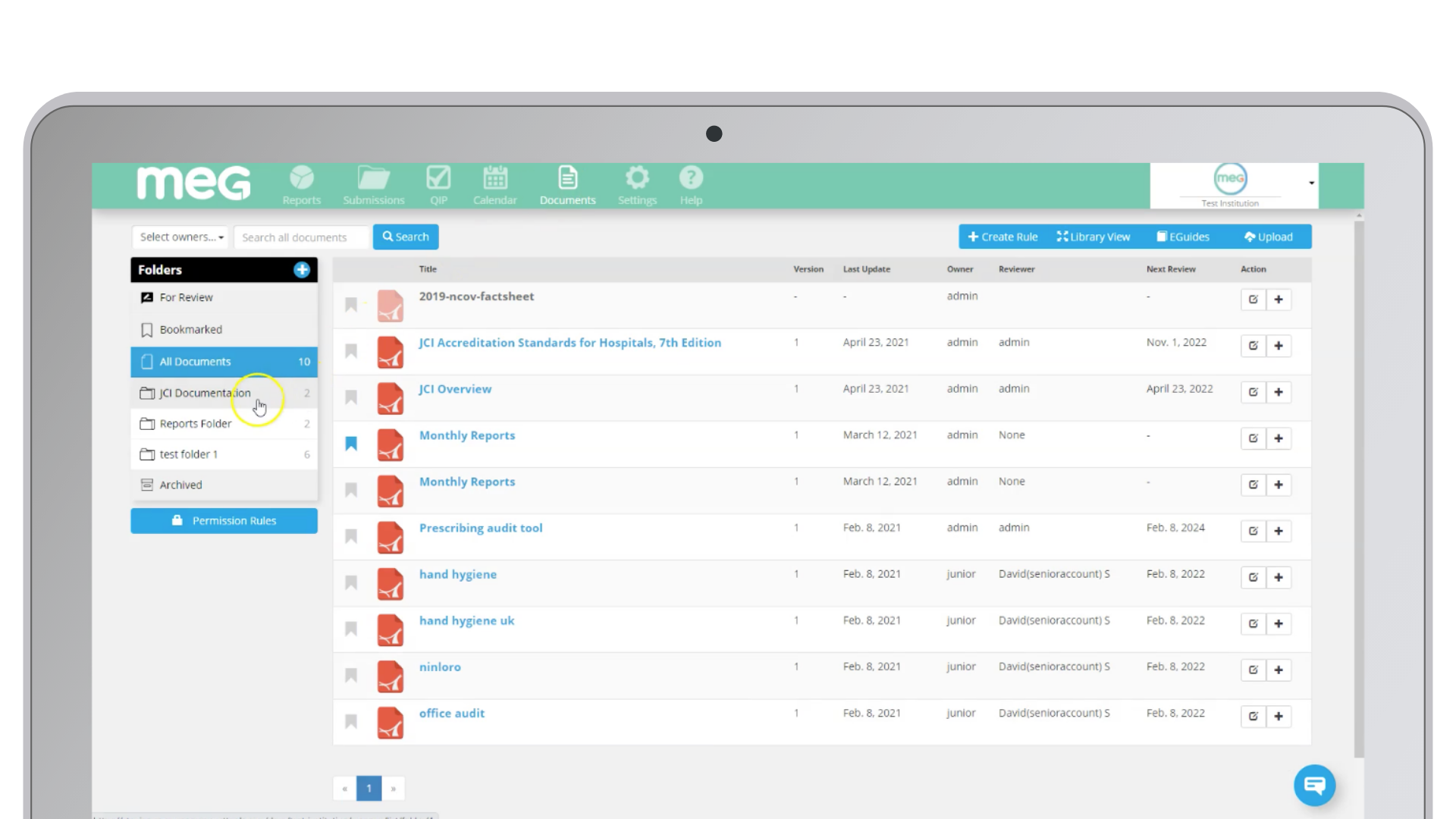
Transformative Technology: Improving Patient Safety
In the digital age, technology plays a crucial role in healthcare improvement. Implementing patient safety and quality systems can make a difference. Through specialised software, effective audits can be conducted, and accreditations of high standards like those of the Joint Commission International (JCI) can be tracked. These systems not only monitor quality but also identify areas for improvement and prevent future incidents.
MEG: Offering Solutions
Through MEG, we present effective solutions to address common challenges in patient safety in the medical field:
1. Medication Management: We offer the Antibiotic Administration Survey to address common errors in medication administration.
2. Surgical Errors: To prevent surgical errors, responsible for 10% of preventable harm, we provide efficient access to the World Health Organization's Surgical Safety Checklist, available digitally in the context of Safe Surgery for Latin America and Spain.
3. Healthcare-Associated Infections: In response to healthcare-associated infections, accounting for 0.14% of cases, we implement measures to reduce antibiotic resistance and control infections in the medical field.
4. Sepsis: Sepsis is a critical concern, with approximately 23.6% of cases occurring in hospitals. We offer specialized audits in infection prevention and control to address this issue.
Looking to the Future
The data confirms that patient safety is a critical priority in Latin America and globally. Preventing and reducing adverse events in healthcare is possible through effective strategies and global collaboration. Our ultimate goal is to ensure that every patient receives safe and high-quality care. Through awareness, a focus on vulnerable groups, robust health policies, a safety culture, and ongoing research, we can move towards a future where patient safety is constant. The adoption of advanced technologies, such as audit and tracking software, will be crucial for continuously improving the quality and safety of care provided. Ultimately, we all play an important role in this process, from healthcare professionals to informed patients, collaborating to achieve optimal and safe care for patients.