Over the last decade, and specifically since the Covid-19 pandemic, society’s need for access to quality healthcare has significantly increased. But unfortunately, a survey by Statista showed that, on average, 40% of the respondents across 32 countries were unsatisfied with their country’s national healthcare system.
In the past, hospital boards and committees had no statutory duty to ensure a particular level of quality when delivering healthcare. However, that is no longer the case. Today, quality and patient safety dominate the clinical governance agenda with board-level attention. And with the latest technological advancements and digital tools at our disposal, implementing a system that focuses on delivering safe, effective, and person-centered care to every patient is easier to accomplish. And that's where a Quality Management System (QMS) designed specifically for healthcare providers comes in.
This post is an in-depth guide to quality management in healthcare. We’ll discuss what a QMS is and its benefits, the implementation process, how to evaluate if a QMS is the right fit for your organisation, how to calculate the ROI, and more.
What is a Quality management system?
Simply put, the generic definition of a quality management system is the organisational structure, processes, procedures, and resources needed to implement, maintain, and continually improve the quality of services or products delivered.
However, in a highly regulated industry like healthcare, a QMS stands for much more than that. Using a quality management system, healthcare organisations can monitor and measure care quality, streamline existing processes through quality improvement, meet compliance and accreditation standards, support quality assurance, and improve overall patient satisfaction.
We will walk you through precisely how in the next sections.
The current state of the healthcare Quality management system
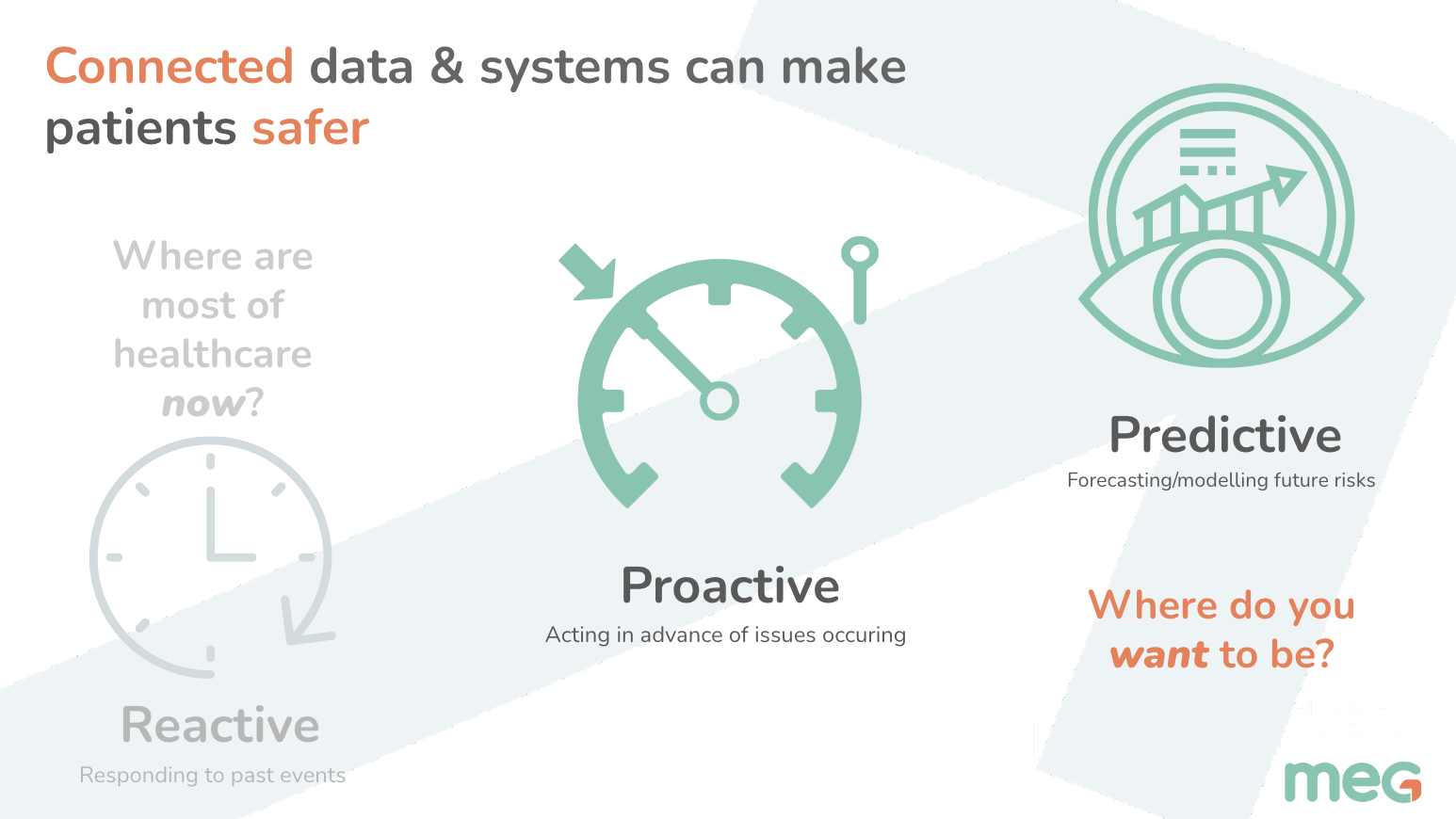
Today, many healthcare institutions use paper or disconnected digital systems to monitor and measure quality. And while this may have worked seemingly well in the past, it simply isn't the way of the future.
With the pandemic accelerating digital transformation like never before, paper-based systems are becoming impractical and increasingly unsustainable. Maintaining an analog system is time-consuming, prone to human error, and leads to a massive amount of fragmented and unstructured data.
In addition, healthcare organisations that use siloed and compartmentalised digital systems for quality management struggle to stay organised amidst the chaos of multiple applications, complicated excel sheets and PDFs.
In the absence of a fully-integrated, centralised platform, data collection, analysis, and reporting become a huge challenge. This fragmented approach to quality management is neither actionable nor proactive, leaving the process of closing the loop between information and action incomplete. Closed-loop visibility? It doesn't really exist.
digital quality management systems: the future IS SOFTWARE
In the previous section, we've established the shortcomings of the systems that most healthcare providers currently use to collect data, analyse it and act on the insights gathered, leaving them feeling like they're flying blind.
And that’s why, today, there is an increasing need for fully-configurable and integrated digital tools that allow healthcare organisations to break down silos, eliminate manual processes, reduce expensive delays, understand care quality, compliance, and patient safety, and improve overall patient satisfaction. That's where the healthcare QMS of the future comes in.
The quality management system of the future is one that goes beyond being simply reactive. It is entirely digital, connecting three main pillars — people, processes, and data. Rooted in a centralised, cloud-based platform that can be accessed anytime from anywhere, this QMS will help streamline processes, accelerate compliance, promote risk-based decision-making, and incorporate tools like Artificial Intelligence and Machine Learning to bring about predictive quality management capabilities.
The benefits of QUALITY MANAGEMENT software for healthcare
A proactive, digital, and centralised quality management system has many benefits. Here are some of them:
1. Increased efficiency:
Outdated systems and manual processes are often complex, time-consuming, and prone to error. This leads to wasting time and resources that could be better utilised elsewhere, ultimately negatively impacting productivity.
On the other hand, an effective QMS boosts efficiency in healthcare delivery by streamlining processes and communication, automating repetitive and administrative tasks, and reducing duplication of effort.
2. Increased consistency:
According to research, inconsistent and undefined processes can have 5x more negative impact on the customer than the delivery of a poor product. And in healthcare, where consistency and quality are crucial, this can have severe consequences.
A good quality management software helps overcome this challenge - it defines all the best practices, policies, and SOPs (Standard Operating Procedures) required to provide quality and consistent care and organises them into a single centralised location. Your staff can then easily access and implement them on a daily basis.
3. Automated and better compliance:
A report by the American Hospital Association (AHA) showed that hospitals, health systems, and post-acute care providers spend over $39 billion annually on administrative tasks related to regulatory compliance. When you break it down, the regulatory burden on a healthcare institution is $1,200 for every patient admitted.
An effective quality management software can bring that number down significantly through automation. For example, apart from cost, MEG's QMS reduces admin burden to a large extent by automating +70% of the audit and incident management processes. As a result, your staff can quickly run audits, review targets, monitor compliance, and tweak processes when needed with minimal effort. Ultimately, this gives you time and resources to implement actual quality improvements within your organisation.
4. Continuous quality improvement:
When using paper or digitally disconnected systems, you're left with a lot of unstructured data.
An effective QMS brings order to the chaos by structuring and analysing large amounts of data, unlocking vital insights previously inaccessible. This information can then be used to identify areas of improvement, proactively address quality issues by implementing new and optimised processes, monitor and track patient outcomes, and continuously make changes based on the results to boost overall care quality.
5. Reduced costs:
There are two main ways through which a sound quality management software can reduce costs:
a. Prevention of adverse events:
According to research in the UK, the total cost to the NHS of preventable adverse events (in extra bed days alone) is around £1bn a year. Further, nearly 15% of hospital expenditure in developed countries is attributable to treating safety failures.
Using a proactive QMS like MEG with risk reporting and incident management tools helps reduce the number of adverse events reoccurring by over 15%. Further, AI-enabled systems with predictive quality management capabilities can provide healthcare professionals with invaluable insights about potential risks, enabling them to make more informed decisions about patient care. The result? Better outcomes and reduced costs.
b. Increased efficiency:
Eliminating capital-intensive legacy quality systems, reducing the duplication of effort, and improving overall efficiency frees up resources to be better utilised elsewhere. In the long run, this can reduce operating costs to a great extent.
THE ROLE OF QUALITY MANAGEMENT SOFTWARE IN high-quality care
When broken down, a digital quality management system includes four main processes. They are:
Quality Planning: Identifying and describing your goals, quality standards, evaluation metrics, processes, and procedures
Quality Assurance: Ensuring the quality of a service or product delivered meets the specified requirements
Quality Control: Ongoing monitoring and support of routine operations, systems, and processes to ensure that they are performing at acceptable levels
Quality Improvement: Capturing opportunities for improvement, tweaking processes, measuring the new results, and sharing the knowledge
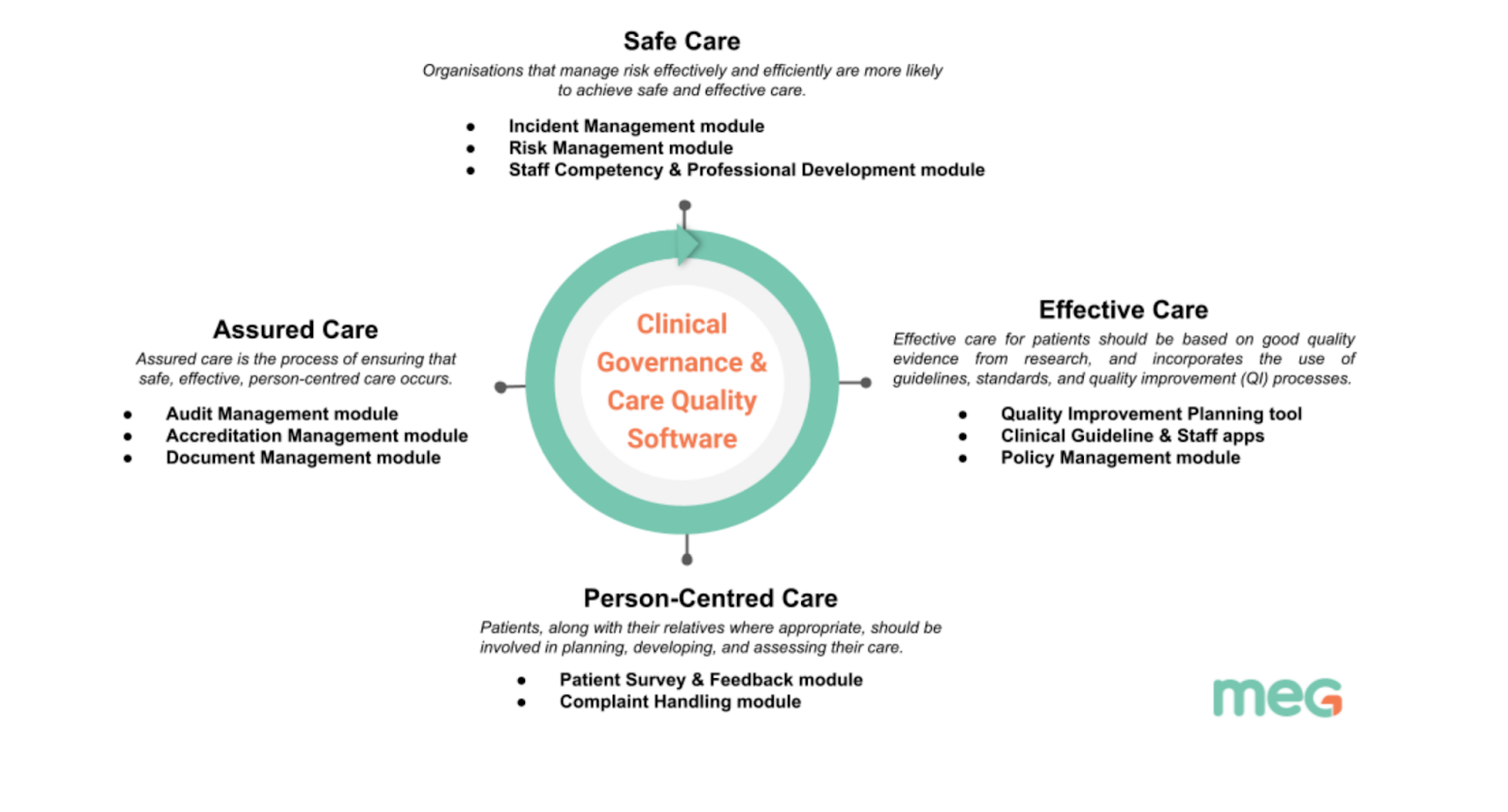
An effective healthcare quality management software connects these four critical components of clinical governance and quality management into a single, centralised platform, allowing healthcare providers to deliver high-quality care i.e., safe, effective, assured, and person-centered care to every patient, every time.
Here’s a snapshot of how the different components of a QMS helps achieve that:
The challenges of implementing a new DIGITAL Quality management system:
Despite the benefits that an effective QMS brings to the table, healthcare institutions are often slow or reluctant to replace their existing systems. This could be because of several challenges, some of which include:
Competing priorities: The healthcare ecosystem is extremely complex, with many stakeholders, such as board members, doctors, department heads, insurers, and regulators playing different roles. Thus, any significant change (like the implementation of a new QMS) must satisfy the varying interests and priorities of all, if not a majority of these stakeholders. And therein lies the challenge.
The cost of change: Eliminating inefficient systems and implementing a brand-new system can be resource intensive, at least in the initial months. This can pose a barrier to change, especially if an organisation does not have the resources (financial or otherwise) needed to allocate to this change.
Staff buy-in: While the C-suite signing off on a new QMS is crucial, staff buy-in is just as important. If your hospital staff are not engaged or committed to the long-term vision of the change being implemented, the chances of it being successful are low.
Apart from this, factors like unstable leadership and technical problems are other barriers to implementing systemic changes. And that's why having a solid implementation plan, and operational roadmap is critical to minimise the above challenges.
In the words of Peter Drucker, “Vision without execution is delusion. The joy is in the results”.
This brings us to our next section…
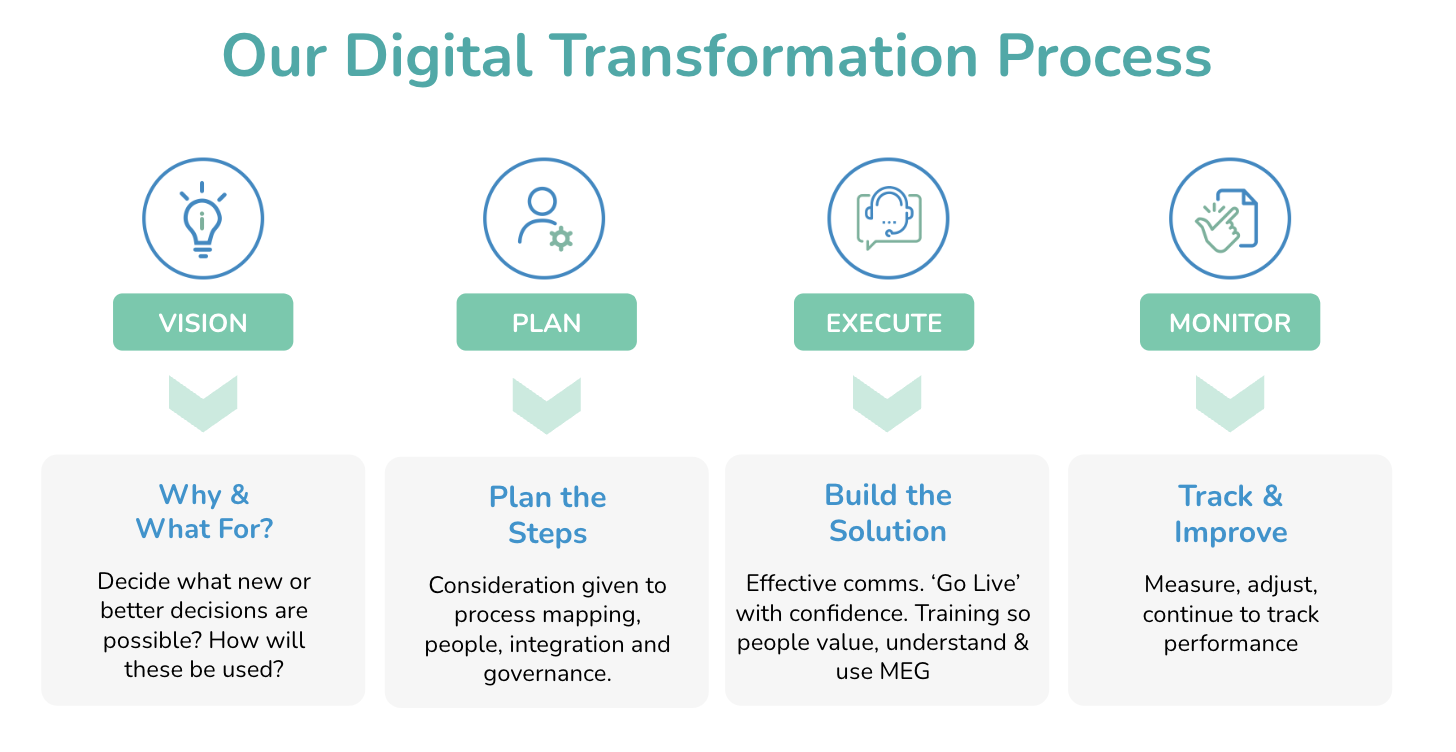
How to implement healthcare Quality management SOFTWARE: From start to finish
At MEG, we break down the end-to-end process of implementing a digital healthcare QMS into four main stages. They are as follows:
STEP 1: Create the vision
Perform an internal audit of your current system
Before implementing a new QMS, it's important to evaluate your current quality system. What are its strengths and weaknesses? Why is it no longer efficient? Are there any features you would like to retain in the new system? You can also conduct a thorough gap analysis of your current processes and where you’d like them to be. The results of this audit will help you determine precisely what’s working with your current system, what’s not, and what functionalities you need in a new QMS.
Visualise your new digital QMS
Once you've evaluated the offerings and shortcomings of your current quality management system, the next step is to outline your ideal QMS. Start by answering the following questions:
What features/functionalities is there a real need for?
What areas within your organisation can a digital QMS address?
How will the implementation of a new QMS improve your existing processes?
What major pain points in quality management does your organisation need to address?
What is the expected output from a new QMS?
Reflecting on these questions will help you identify exactly what you need from a new digital quality management system. In other words, it'll provide you with a clear vision of the way forward.
STEP 2: Plan the strategy
Get management onboard
As discussed in the previous section, management buy-in is one of the main challenges to implementing a new QMS. And that’s why it’s crucial to involve key decision-makers at the beginning of the planning stage. Walk them through your objectives, ideas for the new system, the benefits, and how it will effectively address the existing pain points.
You can even create an execution roadmap and present it to the various stakeholders so they can understand the big picture. This is also a great time to discuss important matters like the budget, resources needed, and implementation timeline to ensure that you're all on the same page. A top-down commitment is key to making a project like this work.
Build the business case for a digital system
Calculating the investment cost for a new quality management system is fairly simple and straightforward. However, assigning a tangible value to the return on investment, especially when measuring factors like productivity, automation, and consistency, can be a challenge.
There's also the question of what will provide better value for your money — building a new system in-house with the help of your IT team or working with a digital partner who can offer an off-the-shelf solution to suit your requirements.
One common way to determine cost-effectiveness is using ROI calculators online to estimate the cost of setting up a new system and the returns in your bottom line. For instance, MEG’s ROI calculator for audit management will help you understand how you can save time and money and improve patient outcomes with a digital tool designed for healthcare organisations like yours.
Choose the right QMS
Today, there is a large selection of QMS providers that you can choose to partner with. However, not all of them may have the features and functionalities to support your organisation’s current and future needs. And that’s why we’ve made a checklist of key factors to look out for in your search for the best QMS. If the answer to most of the questions below is yes, then you’ve most likely found ‘the one’.
Is it specifically designed for healthcare institutions?
Can it be integrated seamlessly with your existing systems?
Does it meet the current needs of your organisation?
Can the system be configured according to your specific requirements?
Does the system take into account user experience?
Is it secure?
Is it simple and easy-to-use?
Does the vendor provide good customer support?
Can the vendor showcase case studies/testimonials from other healthcare organisations using their product?
Does the system provide value for money?
Is the system scalable?
Does the QMS provider offer regular software updates?
Does the QMS provider offer demo/product trials?
We’ve also prepared a product comparison worksheet that you can use to compare different vendors against a set of important criteria. You can download it below.
Once you’ve chosen a vendor and signed on the dotted line, it’s time to get building.
STEP 3: execute the solution
Assemble a team to oversee the project
Over the years of working with healthcare institutions across the globe, we've found that certain elements can really influence successful QMS implementation. And one such factor is the presence of a project management team/person on the client's side to oversee the implementation process from start to finish.
While this isn't an absolute 'must-have', we recommend it for a few different reasons:
Having a team/person as a single point of contact makes the decision-making process and subsequent product delivery timelines quicker.
A dedicated team actively working towards implementing the new QMS and training staff within your organisation leads to a better adoption rate and a higher chance of success.
Set-up a governance process
As you build and execute your new healthcare QMS with your digital partner, it isn't uncommon to want certain improvements or added features (like a new audit).
Rather than immediately reaching out to your vendor and asking them to build it for you, we recommend you take the time to evaluate your ask. Go back to the vision stage and ask yourself — is this feature really needed, will the staff adopt it, and will it make a difference to your organisation's existing quality management process?
If yes, then the project management team can propose it to a body of people within the organisation (preferably those in charge of quality management). Once approved, the requirement can then be communicated to the vendor.
This governance process ensures that you're only building solutions that you're guaranteed to use, in turn, optimising the use of time, money, and effort.
Training and adoption
A crucial part of the QMS adoption strategy is user acceptance testing. Simply put, it is when the quality management system is tested in the real world by the intended audience — in this case, your organisation's staff.
This is where training comes into the picture. While functional and technical training (how to use the different features of the QMS) is something your digital partner can help with, internal awareness training is your responsibility. In a nutshell, this means communicating to your staff the importance of the new QMS, what they should use it for, and how it will simplify your organisation's quality management process.
Equipped with this information, your staff can then test out the new QMS to evaluate if it serves the right purpose in the right way. Bear in mind that not getting enough feedback often means a low adoption/test rate.
STEP 4: Measure and improve
Once your digital healthcare QMS is up and running, it's important to continually measure your performance and capture opportunities for improvement. This, in turn, leads to improved patient outcomes and satisfaction, reduced medical errors and adverse events, improved patient safety, increased efficiency, and better use of healthcare resources.
You can also work with your digital partner to tweak existing solutions and processes to make them even better.
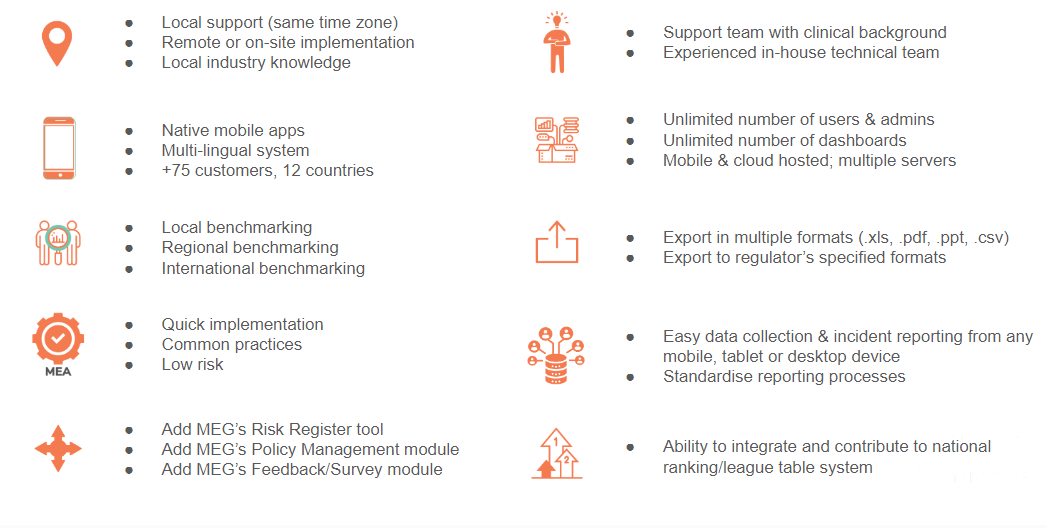
About MEG
MEG was founded in 2016 with the development of its first integrated module - the audit module for healthcare. Since then, it has evolved into a digital, mobile-first, cloud-based healthcare quality management system, connecting people, processes, and data. MEG can be used both online and offline to manage patient safety, compliance, accreditation and quality improvement in an efficient and organised manner.
Here's a snapshot of MEG's QMS and the different solutions within:
Some of our key modules include:
Audit Management
MEG’s Audit Management software replaces paper, spreadsheet, and inefficient auditing solutions with an on-the-go digital system that can be used online and offline. It comes preloaded with audit formats familiar to your team, real-time analytics, task management, and workflows completely tailored to your requirements.
““The MEG Audit tool has made our lives a lot easier in carrying out hand hygiene audits. It’s fast, effective, and saves us time... I would recommend this tool to anyone in Infection Control.”
”
Incident Reporting
MEG's LFPSE-compliant Incident Reporting module helps combat under-reporting by allowing every employee to record incidents in real-time, quickly and accurately. Staff can report concerns on mobile or desktop with our 'quick-capture', expandable incident forms, efficiently manage risk, and gain visibility of incident activity across a single hospital or multiple sites.
““MEG is light, agile and simple to use but gives us robust capabilities for easy reporting at our fingertips.” ”
Risk Management
MEG's Risk Management Solution is designed to help your organisation adopt a consistent approach to assessing and managing risk. It consolidates a range of risk-related activities, the risk register, and documentation such as regulatory standards and local policies into one place, so you have complete oversight at all times. You can also capture incidents and complaints, analyse data through detailed dashboards and heatmaps, plan interventions, and monitor progress.
““ The MEG UI is very easy to pick up and use and the data generated has provided insights which have allowed us to hone in on high-risk issues year on year and show tangible improvements. MEG is shedding light on dark data.””
Document Management
MEG's Document Management tool allows you to securely manage and store policies, operating procedures, standards, and clinical guidelines, in a single, centralised location that you can access on any mobile device or the web. You can also easily search, edit, update and organise documents or share them within teams, departments, and even hospital-wide within minutes.
““We were looking for a user-friendly and adaptable method of getting information to staff in the hospital. MEG has given us the tools to enable us to maintain and update the information locally while knowing that support is there when needed.”
”