Sepsis, a life-threatening condition triggered by the body's extreme response to infection, poses a significant threat to public health globally.
Research revealed that in 2017 alone, there were approximately 48.9 million sepsis cases, resulting in over 11 million deaths worldwide. This staggering toll accounted for nearly 20% of all deaths. Equally concerning is the fact that almost half of these cases occurred in children under the age of five, resulting in an estimated 2.9 million deaths in this vulnerable age group. The burden of sepsis disproportionately affects low- and middle-income countries, where around 85% of sepsis cases and related deaths are concentrated.
Further, according to a recent meta-analysis, there are around 3 million neonatal sepsis cases per year. This means 2,824 cases per 100,000 live births. 84% OF those are preventable.
This blog focuses on the critical importance of preventing sepsis and the role of early detection and treatment, highlighting processes and systems that healthcare institutions can implement to avoid infections and save lives.
Patient Education
Depending on the country and education, sepsis is known only to 7-50% of the people. Most people are unaware that vaccination and clean care can significantly reduce sepsis mortality, even by up to 50%. This lack of education and knowledge is what makes sepsis the number one preventable cause of death worldwide.
Healthcare workers can educate the patient and their family by explaining what sepsis actually is, the causes, risk factors, signs and symptoms, how to take care of wounds to prevent infections, and the importance of antibiotics, vaccinations, treatment, and follow-up care. This can also be done through brochures, pamphlets, videos, and community education programs.
Infection Control
Infection control is the cornerstone of sepsis prevention. However, in Europe alone, approximately 80,000 hospitalised patients are believed to have at least one healthcare-associated infection daily, leading to 16 million additional hospitalisation days each year. Similarly, in the US, HAIs account for an estimated 1.7 million infections and 99,000 associated deaths each year.
In 2022, the commitment of G7 health ministers and leaders to advance sepsis prevention, alongside efforts to combat antimicrobial resistance and enhance infection prevention and control programs, marks a significant stride in the battle against sepsis in Europe. WHO has also collaborated closely with Member States and partners to elevate the standards of infection and sepsis prevention and treatment in Europe.
Healthcare facilities must have stringent infection control protocols in place, including hand hygiene, proper sterilisation of equipment and medical devices, and strict adherence to aseptic techniques during medical procedures to prevent sepsis. Organisations must also establish rigorous cleaning and disinfection protocols for patient rooms, equipment, and common areas.
Apart from this, when performed regularly, infection prevention and control audits help organisations establish a governance process and identify issues, trends, and areas for improvement. This data can then be used to drive continuous quality improvement and reduce the rate of HAIs.
Antibiotic Stewardship
While prompt initiation of antibiotics to treat infections prevents sepsis and saves lives, 30% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or suboptimal.
Antibiotics have serious adverse effects, occurring in roughly 20% of hospitalised patients. Patients unnecessarily exposed to antibiotics are at risk for these adverse events with no benefit. The misuse of antibiotics has also contributed to antibiotic resistance, a serious threat to public health.
Antibiotic Stewardship Programs (ASPs) can help clinicians improve clinical outcomes and prevent the development of antibiotic-resistant infections. Healthcare providers should prescribe antibiotics judiciously, based on clinical guidelines and cultures, and avoid overuse or misuse. It is also important that patients receive the correct dosage and duration of treatment.
Check out MEG's Digital System to efficiently track and report antibiotic use here.
Early Detection
While vaccination, proper hygiene, and emergency treatment play crucial roles in preventing sepsis, early detection remains paramount in reducing its devastating effects.
The statistics and real-world examples we explored in this blog underscore the pressing need for action. With millions of lives hanging in the balance and the burden of sepsis disproportionately impacting vulnerable communities and low-income countries, implementing a system that strengthens early detection, diagnosis, and treatment protocols in every organisation is an absolute necessity.
Early Warning Systems:
The Early Warning Score (EWS) is a physiological scoring system based on signs like core body temperature, heart rate, respiratory rate, blood oxygen saturation, etc., used to evaluate the level of a patient’s clinical deterioration.
This system can be used by healthcare staff to identify patients at risk of sepsis, trigger a clinical assessment, and provide timely care in the form of antibiotic therapy, IV fluids, and addressing the underlying source of infection.
EWS systems also facilitate documentation and communication among healthcare teams. They provide a standardised way to communicate a patient's deterioration or potential sepsis risk, ensuring that appropriate actions are taken promptly.
MEG's Deteriorating Patient Bundle
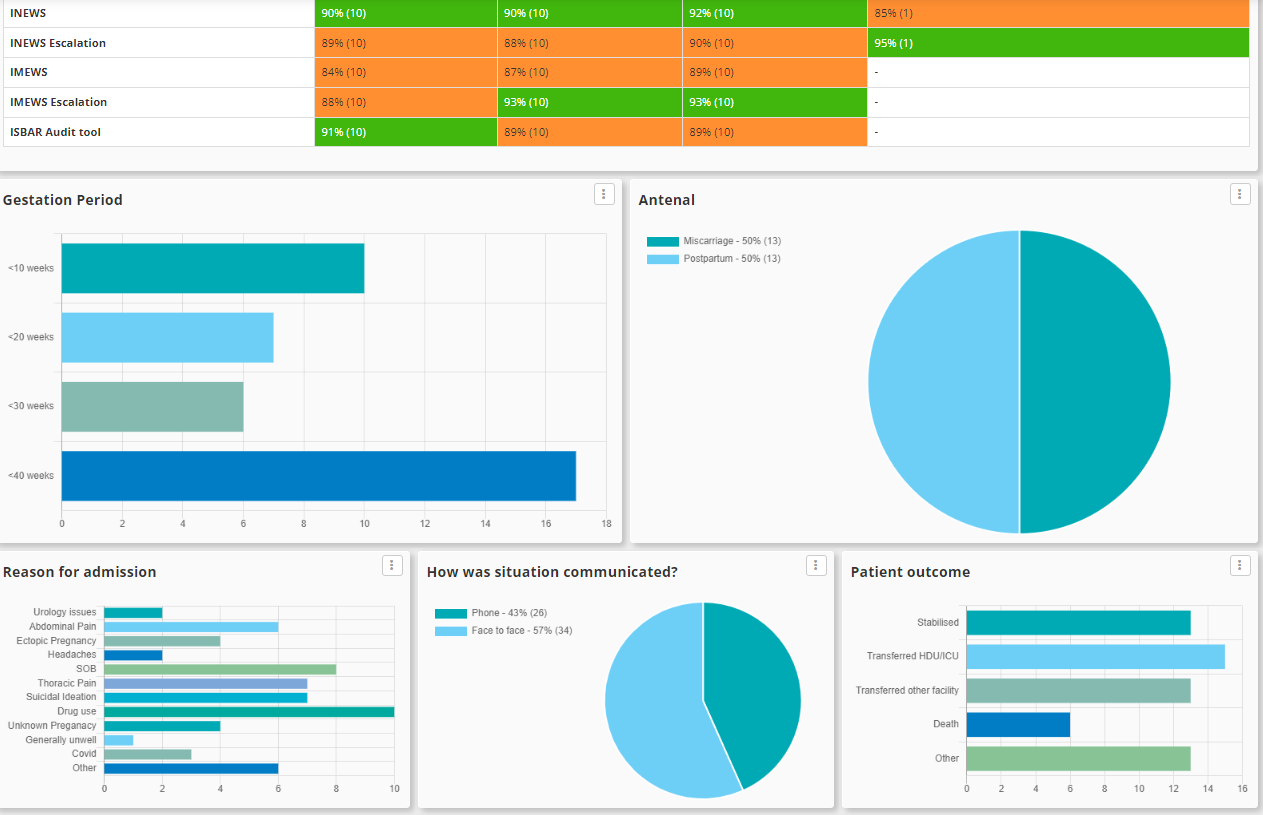
To help organisations with their quality assurance process for patient deterioration, we've put together a collection of assessments and audit tools, including various Early Warning Score forms such as standard, paediatric, maternity, and emergency medicine, each tailored to specific patient populations. The bundle also includes associated escalation pathways following the ISBAR model.
These are governance audits that organisations can use to ensure that their processes are working as designed and that staff are following the necessary protocol to prevent patient deterioration and the likelihood of events such as sepsis.
It also comes with a Quality Improvement Plan (QIP) tool to identify and address any issues or gaps in the assurance process. Here's a glimpse into what the system looks like:
To know how MEG’s Patient Deterioration Bundle can help your organisation, get in touch.