Accelerating safety with clear focus, responsibility, and prompt action.
Healthcare leaders understand that technology alone doesn’t make systems safer. What really counts is how innovations are used to provide staff with clarity, reinforce responsibility, and enable swifter responses. Here are three areas where providers are already experiencing measurable improvements.
1. Digitised Global Trigger Tool (GTT) Reviews
From paper delays to real-time learning
The Global Trigger Tool (GTT), developed by the Institute for Healthcare Improvement (IHI), uses “triggers” - cues in patient records such as lab results, medications, or readmissions - to flag potential adverse events that might otherwise go unnoticed. Traditionally, GTT reviews have been manual and paper-based, taking weeks or months to complete.
A 2019 study in the International Journal for Quality in Health Care found that reviewing 1,000 records with the original manual GTT took 411 hours. With a digital approach, the same review required just 23 hours; that’s a 95% reduction in time (1). That’s the difference between waiting months for insight and having actionable findings in days.
➡️ How MEG helps:
MEG’s Digital GTT module uses AI-powered trigger detection (via Gemini) to scan records and categorise potential adverse events in seconds.
Quickly consolidates data from your EHR or other patient systems, even through a simple Excel upload, so leaders can access insights without waiting months for complex integration projects.
Supports customisable trigger lists, so hospitals can tailor reviews to their services (e.g. obstetrics, oncology)
Provides live dashboards and action-tracking, giving leaders immediate visibility of themes and responses.
💡 Leadership lever: Faster, more consistent reviews free up hundreds of hours of clinical time and bring potential harm signals to safety committees while action can still be taken, strengthening governance and continuous improvement.
2. Keep Safety Actions on Track Automatically
From static logs to proactive prevention
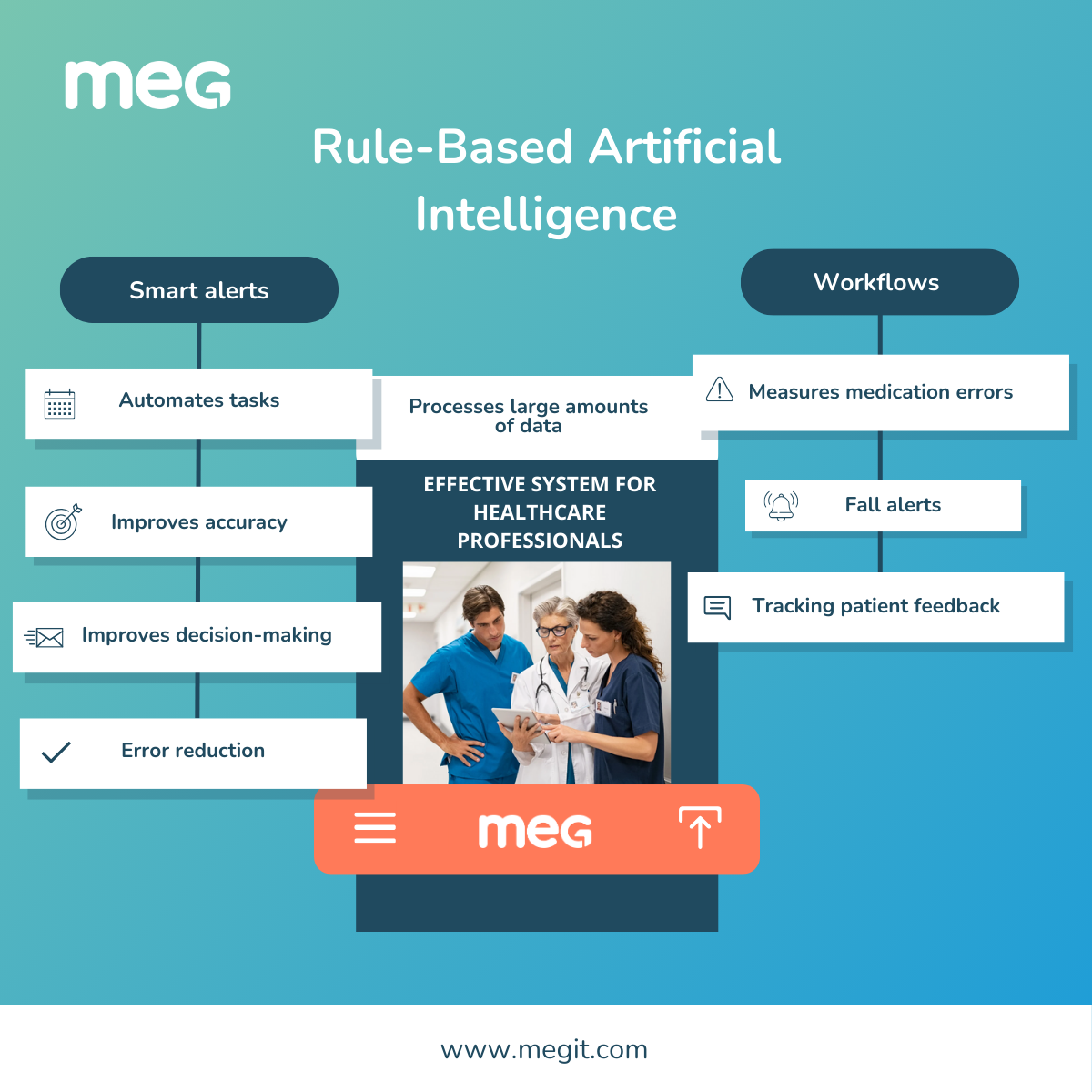
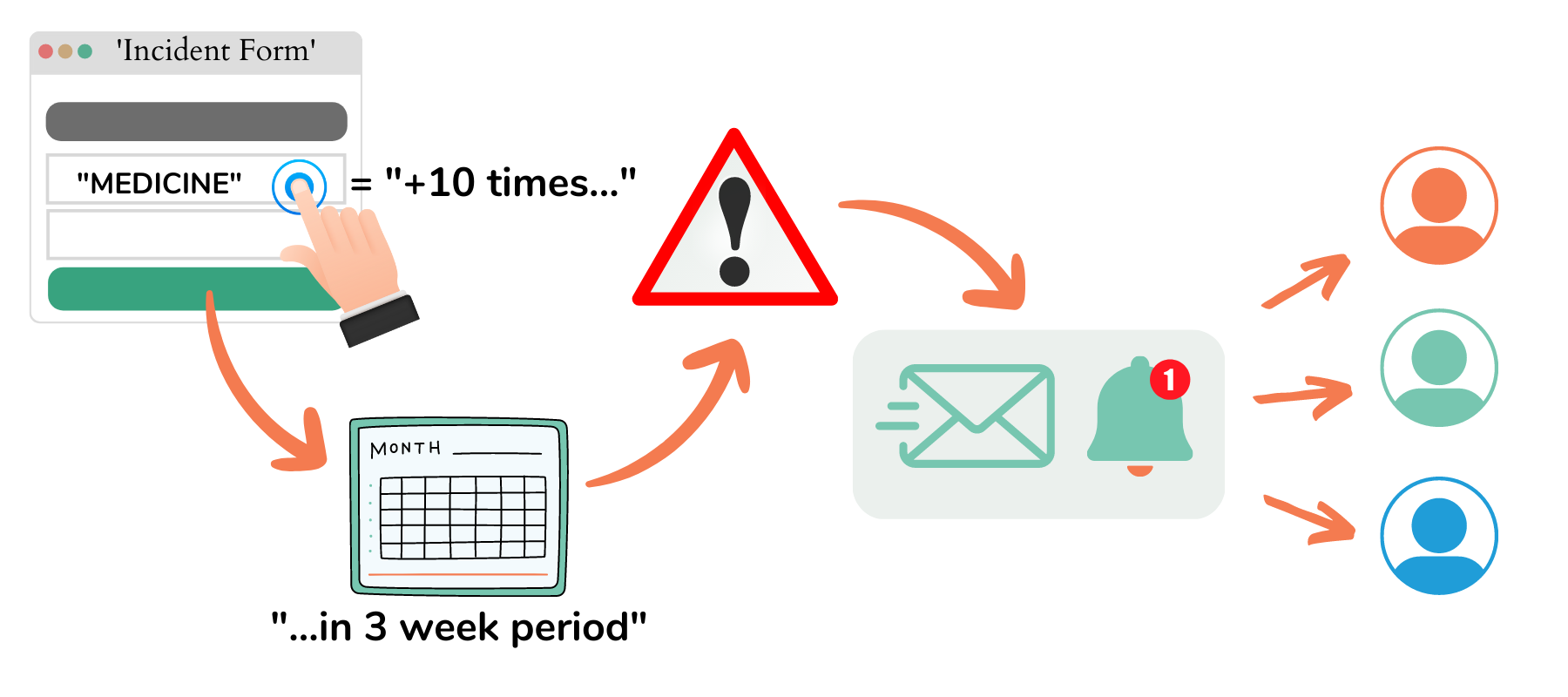
The real risk isn’t just unreported incidents; it’s reported issues that never get resolved. Manual spreadsheets and emails make follow-up hard to monitor, leaving leaders in the dark. Smart, rule-based alerts and automated workflows change that.
➡️ How MEG helps:
Assign actions immediately at the point of review, so ownership is clear from the start.
Smart alerts and threshold triggers keep teams on track, while Red/Amber/Green flags make overdue or at-risk items visible at a glance.
Automated escalations ensure nothing gets lost or delayed.
Board-level KPI dashboards display real-time closure rates across departments, giving executives constant oversight.
Providers using MEG have reported significantly reductions in average closure times in the first six months. At one pilot site, introducing automated escalations cut average ‘actions’ closure times by over 70%, a tangible leap in responsiveness.
💡 Leadership lever: Leaders can track closure rates as a live quality indicator, ensuring risks are not just logged but actively resolved, building accountability and resilience.
3. Turn Gaps and Feedback into Early Warnings
From fragmented data to proactive risk insight
Incidents show where harm or near misses have already occurred. But compliance data, risk registers, and patient complaints often highlight risks before they escalate into incidents. The challenge is that these sources are usually siloed. When they’re connected around a common identifier - such as a patient number, staff ID, or service area - leaders gain a clear, unified view of where vulnerabilities are emerging.
➡️ How MEG helps:
Connect the dots with a common identifier: link compliance checks, policy compliance, training records, and complaint themes directly to incident data.
Spot patterns quickly: dashboards reveal where compliance gaps overlap with incident trends, acting as early warning signals.
Enable proactive decisions: department-level views help local leaders take corrective action, while committee-ready reports provide system-wide oversight without extra admin.
💡 Leadership lever: By linking disparate data sources, boards and safety leaders gain visibility into the underlying drivers of risk, making it possible to intervene early and prevent issues before they result in harm.
Moving Forward
These innovations are not distant possibilities. They are already being used in leading healthcare organisations. By digitising reviews, automating follow-up, and connecting risk, compliance, feedback data (and more!), leaders are seeing faster insight, stronger accountability, and measurable improvements in patient safety.
👉 Want to explore how healthcare leaders are applying these innovations? Join us at any upcoming conferences we’re attending, or connect with us to share lessons learned and approaches that are working in practice.